Warning: What follows is long. It breaks all the normal rules of conventional blogging. It is probably best-suited to those who:
- Have recently been diagnosed with cancer and are living in basic freak-out mode.
- Have a loved one who has been so diagnosed.
- Are either curious about cancer or want to know about the medical, emotional, familial roller coaster I have been riding as of late.
Cancer #1
In 2014, I wrote a blog piece called “Prostate Cancer in the Rearview Mirror.” (See https://blog.livestrong.org/prostate-cancer-in-the-rear-view-mirror-472e135b8191) It explains my journey with prostate cancer from a February 2011 diagnosis to a May 2014 radical prostatectomy and its resulting pathology. In between, I practiced what the Average Jane/Joe calls “watchful waiting” and the intelligentsia refers to as “active surveillance.” (Should cancer enter your life, get ready for a lot of “rose by any other name” talk.) The 2014 piece expresses two-fold gratitude for: 1) the love and support I received from family and friends; 2) the expert and thoughtful care I received from Dr. Francis McGovern and his urology team at Boston’s Massachusetts General Hospital.
A few months later, the blog post wound up on the Livestrong website. Before long, I started getting out-of-the-blue calls from Livestrong readers. Many of these were recent cancer-diagnosed athletes and outdoor enthusiasts seeking the fastest way to get back into their sport or activity of choice. (Note: I had happily noted in my article that I had been able to play in my beloved Lake Placid, NY Grand Masters Lacrosse Tournament just inside three months following surgery.) These calls were not only enjoyable, but they also allowed me, a lifelong teacher, to practice my craft outside of the typical classroom.

At one point during this period, Dr. McGovern pulled me aside and thanked me for being his number #1 source of referral at that time. Sensing my immediate puzzlement, he explained, “We always ask new patients how they heard of our practice. Lately, we’ve been hearing a lot of ‘Some guy from Maine wrote glowingly of you and your team in a blog piece on Livestrong.’” Although surprised by this unintentional outcome, I was more than happy to be helpful to the potential patients of a doctor who had been so helpful to me.
I spent the rest of the 20-teens decade happily, maybe even blithefully, cancer-free. Aside from the support I extended to various friends who had been diagnosed with prostate cancer, my overall take on cancer was pretty much “been there, done that.”

I had hit my 60s and life was good. I had remained active in “geezer” lacrosse tournaments, ran, and played a lot of hoops. I had also taken up stand-up paddling, twice competing in Sea Paddle NYC, a 26-mile circumnavigation of Manhattan that raises big dollars for a cause near and dear to my heart: autism research. (FWIW, both times I think I was the oldest participant.)
The 2020s got off to a great start with our two daughters planning marriages to great guys and our son, an adult with autism, moving into his own home, excited to begin his life independent of his parents.
Cancer #2: “Could you please tell me where the restroom is?”
A year or so into this decade, it dawned on me that I was urinating more often than usual. It took a while to sink in, perhaps because the Covid pandemic was top-of-mind, but the seemingly constant need to urinate ultimately began to take up too much space in my life:
- Whenever I went into an unfamiliar building, I would check for bathrooms.
- During meetings at work, I would always try to secure a seat closest to the bathroom.
- My thrice-weekly basketball games involved several exits to relieve myself while my fellow senior citizen players never seemed compelled to leave the court.
What’s more, the extent of the output seemed strangely at odds with the intensity of the urge. In other words, I’d be absolutely dying to urinate, but upon finding a bathroom (or a suitable outdoor substitute), a mere ounce or two would slowly trickle out of my body. After living with this for over a year, I set an appointment with Dr. McGovern.
Before that appointment was over, I learned that I likely had bladder cancer.
Just as my journey with prostate cancer introduced a whole bunch of strange new words and terms – e.g., Gleason score, PSA, radical prostatectomy – my second glossary tour of the Big C began when Dr. McGovern said, “I think we ought to do a cystoscopy.”
Not knowing the meaning of that term, I offered, “OK. Do I schedule it with the front desk?”
Dr. McGovern replied, “No. Let’s just do it right now.”
Having put my life in the hands of this amazing physician before, I said, “Sure.”
Next thing I know, a local anesthetic had been applied to my privates and a few minutes later, Dr. McGovern and I were watching a movie starring the inside of my bladder. Incredible, to say the least. To make this happen, a microscopic camera, equipped with a microscopic flashlight, is placed at the end of a microscopic tube. (To save time and words, let’s just say there’s a whole lotta “microscopic” goin’ on.) Then Dr. McGovern’s steady hand guides said tube up the urinary tract – as in, my urinary tract! – until it reaches the bladder and takes a look around. All of this is projected live on a computer screen for the viewing enjoyment of the doctor and patient.
Needless to say, I had no idea what I was looking at. Before long, Dr. McGovern enlightened me with, “Well, I can see at least one reason why you’re urinating so much. You’ve got a good size tumor, and the bladder is a very small organ. So, there’s less space for storing urine.”
“Bladdih Cansah?”
Before the appointment was over, plans were made to schedule a TURBT surgery. I can never remember what those letters stand for, but my takeaway from Dr. McGovern’s explanation was that the procedure involves all the components involved in the cystoscopy with one addition: a microscopic… See, what I mean?… scalpel connected at the end of the whole ensemble that shaves off the tumor. While taking all of this in, I made a silent vow to never again make fun of science geeks. While Dr. McGovern never used the word “cancer” – No way to know for sure until the tissue is examined – that vibe was in the air of our conversation.
Back out at the front desk, I noticed another patient waiting. Standing next to a woman (girlfriend? wife?), he was wearing work clothes and a labor union t-shirt. My first reaction was that it reminded me of yet another reason I hold Dr. McGovern in such high respect. When you visit his office, you are as likely to see a white collar State Street banker (or maybe a professional athlete) as you are a blue collar worker. My second reaction: This guy is trying to get my attention. When our eyes met, he spoke/whispered a two-word question across the room in an accent that maybe only Ben Affleck or Matt Damon could mimic: “Bladdih Cansah?”
Caught off-guard, I muttered something to the effect of, “Looks that way.”
He replied, “This is my fourth time around with bladder cancer and Dr. McGovern. It ain’t as bad as it sounds. Let me walk out with you and we can talk.”
Open to any support I might receive, I followed him and his significant other out the door. No sooner had we gotten outside when he pulled out a pack of Marlboros, offered me one, handed one to his partner, put another one in his mouth, lit both of them up, and exclaimed with a sigh, “You can’t smoke anywhere these days!”
Startled by their decision to smoke in the midst of our particular circumstances, my insides were screaming, But aren’t cigarettes, like, the #1 cause of bladder cancer?!? But I held my tongue, open to learning any wisdom he might impart about what the future might hold.
After some supportive talk, he shook my hand, wished me well, and said, “Hey, we’re heading to a bar (bah) just a block away. It’s called Harvard Gardens (Hahvid Gahdins). We always go there after my appointments with Dr. McGovern. Sometimes to celebrate. Sometimes to drown our sorrows. Either way, it’s a good time. Stop by later if you want. We’ll be there a good while.”
I didn’t tell him that I had stopped drinking in 1985 and smoking two years before that, but I appreciated his thoughtfulness and generosity of spirit. In my experience, that’s pretty typical behavior of cancer patients. We appreciate support and most of us pay it forward. That guy put me at ease. And he came along at just the right time. Have not seen him since. Hope he’s well.
May 16, 2022 – TURBT Surgery at Mass General
A few weeks later, I’m back at MGH, sitting up in a hospital gurney bed. I had just been given my anesthetic. I’m starting to drift off into la-la land. A group of nurses, doctors, and various helpers are gathered around me. And then Dr. McGovern announces to all present, “This man is a teacher who has touched and saved thousands of lives. And he’s not done. We need to take care of him so that he can take care of thousands more!”
Then, with everybody applauding me, Dr. McGovern grabs the handle on the gurney and proceeds to wheel me down the hallway to the operating room. It was so deeply touching and special that I felt like I was down the street at the Fleet Center getting introduced in the starting line-up for that night’s Celtics game. Don’t remember much else. I might have even gone down for the count before we even reached the operating room.
A few hours later, Dr. McGovern tells me that the operation was a success. He explains that I will have a catheter for a few days and that he would walk me though the process of removing it via video chat. Before I knew it, I was on my way back to Maine.
Having had a catheter following my 2014 radical prostatectomy, I was familiar with the process. It’s not anyone’s idea of fun, but, Hey, you don’t ever have to get up to urinate! That weekend, Dr. McGovern called me as promised and coached me through the removal of the catheter. Although I had some trouble passing urine during the next 24 hours, that hiccup quickly passed.
A week or so later, Dr. McGovern called me with the bad news that, as expected, the tumor in my bladder was indeed cancerous. The good news was that he seemed confident that the tumor had been fully removed without any damage to my bladder.
Follow-Up Treatments
Once the inside of my bladder had heeled – about a month following the TURBT procedure – I began a scheduled routine that alternates immunotherapy treatments with check-up cystoscopies. This is to ensure that the cancer does not return. We kicked off with a regimen of six weekly 10-minute immunotherapy treatments where a few ounces of Bacillus Calmette–Guérin (BCG) is injected directly into the urinary tract. (I digress: It takes a while to accept the idea that that tiny hole at the end of one’s penis is not just an exit door for secreting fluids. It can also double as an entrance door for healing fluids. Graphic maybe, but I assure you that imagining it is not as disturbing as actually experiencing it!) Then the BCG settles in the bladder where it stays for two hours when the patient then urinates it out.
Whenever I tell people about this, they invariably respond with something like, “Oh, you mean, chemo?” No. My laymen’s understanding would put it this way: Whereas chemo acts like Drano, BCG acts as a reinforcer to those enzymes in your body that fight cancer. (Note: Originally intended as a treatment for tuberculosis, doctors stumbled over the discovery that BCG could also be very effective as an antidote to bladder cancer.) In my case, cancer had been winning the battle and reinforcements were needed. Enter BCG.
A month or so following that initial regimen of six weekly BCG treatments, Dr. McGovern’s follow-up cystoscopy showed no return of cancer. From there, we went to a quarterly regimen of three weekly BCG treatments followed by cystoscopy. After Year #1, we will transition to every six months. Then we will transition to an annual routine.
Thankfully, Dr. McGovern arranged for me to have the majority of my BCG treatments at Fore River Urology in nearby Portland (ME), saving me the hassle of having to drive to (and park in!) Boston every week for a 10-minute appointment.
Of course, this schedule assumes that I remain cancer-free throughout. Should the cancer return at any point, options might include a second TURBT. (Note: This can be risky due to the fact that the bladder is a very sensitive and fragile organ.) Another option is the installation of an artificial bladder. Obviously, I am hoping for the best, but if I have learned anything, it is that cancer cares nothing about my hopes.

Heavy Traffic – A Roundabout of Birth, Death, and a Wedding
There are at least three reasons why my Cancer #2 diagnosis was less of a freak-out than Cancer #1. For one, I’m a second-timer and I had already forged a profound trust in and respect for Dr. Francis McGovern and (everyone I encountered at) Mass General.
Another reason has to do with Laura’s (my wife of 44 years) diagnosis with breast cancer a few months before. Supporting her through her surgery and treatments at Brigham/Dana Farber likely helped me defer my anxiety and fears about my own situation. (Thankfully, Laura is now in full recovery!) Sometimes the best way to help yourself is to actively care about somebody else.
Third, I learned during Cancer #1 that worry is a counter-productive emotion. (Of course, that does not mean that I never indulge in it!)
However, the biggest difference between Cancer #1 and Cancer #2, is that the latter has occupied my life during the toughest stretch I have experienced in my 69 years. Less than two months after my TURBT, we lost Harrison, our only son. While swimming at Maine’s Sebago Lake with his caregivers – they were actually wading in chest deep water – he had a seizure, took in too much water, and could not be revived. As I write, our whole family remains overwhelmed with grief. In fact, upon hearing the news, I became so totally unglued with trauma that I required an ambulance ride to Maine Medical Center. (That was my second hospital trip that day as I had had a BCG treatment that morning.) Six months later, tear-triggering memories are a daily part of our lives.
On the one hand, I’m evolving to a point of placing my highest gratitude on the 28 years we had with Harrison while trying to let go of the additional decades we will never have. On the other, I know I’ll never get over this loss. At this point, I don’t even seek that as a goal. I write about it here because, well, it’s the biggest plotline in my story.
Early on, a cancer patient learns to accept that, post-diagnosis, life goes on. After a while, you even wrap your brain around the idea that sometimes it does not go on. Cancer or not, nothing prepares you for the loss of a child. As I said at Harrison’s memorial, “For me, the only thing worse than writing your own child’s obituary is the thought of having somebody else write it.”
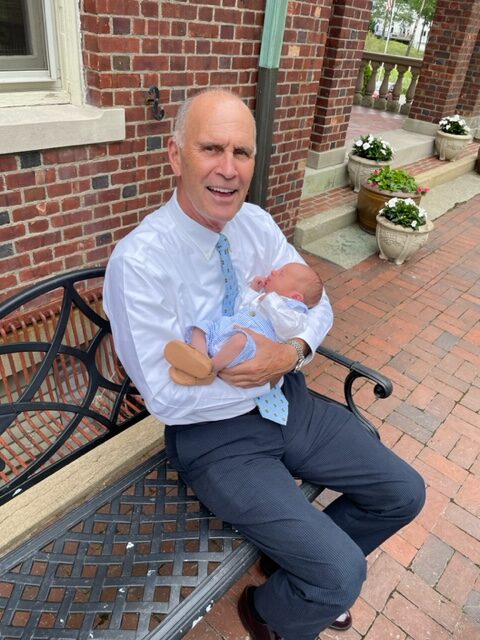
A week after Harrison’s death, Laura and I were blessed with the birth of our grandson, our first grandchild. At the intersection of that intense yin of birth and yang of death, we were also in the midst of planning our second daughter’s wedding less than a month away. When we sat down as a family to discuss the possibility of postponement, there was immediate unanimity to proceed as planned. We knew that Harrison would have insisted we keep on keepin’ on. He did that throughout his life. We’re following his example.
For my part, I continued to follow my treatment schedule. Discussions with my wife, my daughters, and Dr. McGovern, who demonstrated a depth of interpersonal connection matching his surgical skills, helped me see that I would be no good to anyone else if I did not take care of myself.
It was an awesome wedding. When we weren’t dancing, we were playing with our grandson. And Laura and I have since been doing that at every opportunity!
Finally, there’s a substantive difference between this story and the 2014 “Prostate Cancer in the Rearview Mirror” piece: This cancer is not in the rearview mirror. Last time, I did not want to write anything until I was in the clear. This time around, I’m seeing that either “the clear” is a mirage… OR… objects in the rearview mirror are most definitely closer than they appear. Either way, keep your eyes on the road ahead.
Onward, Malcolm Gauld
PS: While putting the finishing touches on this post, my dad — Joseph Gauld — passed away at age 95. Suffice it to say that this event has contributed to the aforementioned emotional maelstrom in ways I do not currently comprehend. Please join me, our family, and friends on June 10 (3 PM) at Hyde School as we gather to celebrate his life. And what a life it was!