Greetings! Well, my condition is much improved since my last post. Legs are getting back to normal. Complications continue — You know how it is: a blood clot here, a positive test for “Type A Flu” there — but enough about me…
Continuing in “once-a-teacher-always-a-teacher” mode, thought I’d share 5 of the biggest lessons I’ve learned during my 15-year journey with cancer.
1. The more accomplished/cutting-edged/prestigious the doctor… the more likely their prescribed treatments will be out in front of the insurance approvals.
A couple months after my 11/24 radical cystectomy, it was time for the follow-up treatment. My oncologist prescribed the cutting-edge Niagara Protocol. (Nutshell: a chemo/immunotherapy combination) At the time of prescription, the Niagara Protocol had been approved for lung cancer and was in the consideration phase for bladder cancer. (BTW, It’s expensive. About $1M for the whole shebang.) Doc cautioned me to expect to be turned down on the 1st request. (We were.) He then went back at it hard, but we were turned down again. He said, “Not to worry, I have quality substitutes in mind that will be approved.” (They were.) We did said substitutes and I’ve had two clear CT scans since then… Post Script: Two months into my treatment, I read that the Niagara Protocol had been approved for bladder cancer. Yeah, my doc was/is ahead of the curve. Hence, quality care is not without complications.
2. If you opt for a major hospital 2+ hours from your home setting… do not burn your bridges with your local doctors.
You will be hard-pressed to find a bigger cheerleader for Mass General than me. MGH is also 2+ hours from my home. (And that’s if you get lucky at the Tobin Bridge.) Over the years, I have known fellow Mainers with significant health issues who, like myself, have opted for one of the major Boston hospitals. I’ve heard some of them bad-mouth or look down their noses at Maine doctors and facilities… Bad move… Urgent needs have a way of rudely popping up out-of-the-blue. (That’s why they call them “urgent.”) My own recent short list would include abdominal discomfort, ultra-sounds that detected the blood clot I acquired last month, and the “A Flu” virus I caught last week. When these things do pop up, you need a committed local team in your corner. And it’s on you to be a great captain to that team!
3. “Regardless of how sophisticated the surgical procedures or medications may get, nothing beats early detection.” – Dr. Francis McGovern, MGH Urologist
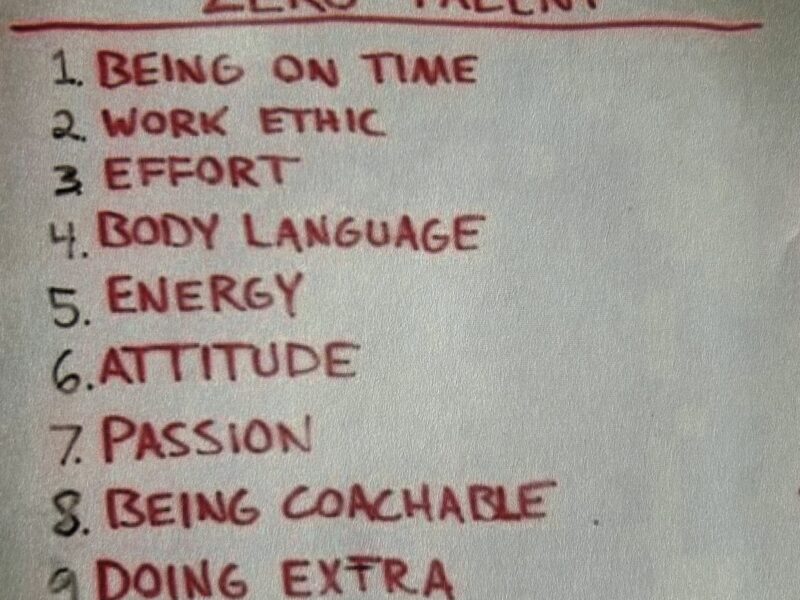
Cancer has taught me that I’ve spent too much of my life worrying about things that don’t matter all that much. If you are putting off any health check-ups or tests — e.g., colonoscopies, PSA tests, yearly check-ups — know that you’re doing the same thing. So: a) Knock it off; and b) Get with the program!
4. Transcend the “Availability Heuristic.”
I’ve referenced the availability heuristic in past email blasts. Here’s a definition I lifted off the internet: “a type of mental shortcut that involves estimating the probability or risk of something based on how easily examples come to mind.”
Both cancer and its array of treatments are like snow flakes. Just because Uncle Bob or Aunt Jane had a particular cancer and: a) survived/thrived; b) died; c) had a terrible treatment experience; d) acquired yet another cancer, etc… does not mean that you or anyone else are destined to the same fate. I’ve encountered a number of people locked into a myopic understanding guard-railed by the personalities they may happen to know who have or have had cancer. So, be conscious of your cancer biases and transcend, deepen, and broaden your understanding. It could save you or someone you love.
4. b. As an addendum to Point 4, let me stick it just a bit to you men out there:
In 2015, I wrote a blog post called “Prostate Cancer in the Rearvew Mirror” that wound up on the Livestrong website. (True Story: A few months later, my MGH urologist told me that I had become his #1 source of referral. Had no intention of referring anyone when I wrote it!) Anyway… Here is an excerpt from that 2015 Livestrong post:
I began to perceive a sharp divide between men and women regarding their approaches to cancer… Whether participating in a Run for Breast Cancer or sporting pink lapel ribbons, women didn’t emanate the secrecy that shrouds men and prostate cancer. On more than a few occasions I came across longtime buddies who had experienced prostate cancer, and I had never known it. (At my 40th high school reunion, on the second fairway of a golf course, three of us in the same foursome were more than a little surprised to discover that we shared club membership in common.)… In the end, I can’t say how open the average guy should be about his prostate cancer, but I can say that I was struck by the difference men and women seem to reflect when it comes to living with their respective cancers. Part of the reason I am writing this piece at all is because I had hoped that some open sharing might be useful to others in this position. I would say that it’s the women I have known with cancer who have taught me to see it this way.
5. Accept and embrace the uncertainty.
Doctor’s explanations of your status as a cancer patient will never be as complete as you will want. You — and your loved ones — are always going to want more info than you get. Let go of that “need” and replace it with some one-day-at-a-time serenity. Speaking for the uncertainty in my own life, I’m hoping that I’ve got a good ten+ years ahead of me, but I accept that I may not have 10 months. I’m just focused on making sure that each and every day going forward will be awesome. Come to think of it, that’s a good plan for… anyone.
Onward, Malcolm Gauld
PS: If you’re interested, here’s the link to that 2015 Livestrong piece:
https://medium.com/livestrong-voices/prostate-cancer-in-the-rear-view-mirror-472e135b8191